
Patients with nasogastric suctioning lose H + produced by gastric parietal cells. ECF volume contraction and hypokalemia maintain metabolic alkalosis once it has been initiated. Vomiting and some forms of chloride-containing diarrhea cause proton loss and subsequent HCO 3 – generation. Redistribution of H + from ECF to the ICF may also result in metabolic alkalosis. Patients may present with acid loss due to extra-renal or renal H +wasting. Hypercalcemia and vitamin D excess increases proximal renal HCO 3 – reabsorption. In some Asian countries, betel nut chewing can cause this problem due to excessive calcium ingestion. It presents with nephrocalcinosis, declining renal function and metabolic alkalosis. There is a rising incidence of milk-alkali syndrome especially in women taking calcium supplements for osteoporosis. Following treatment of lactic acidosis or ketoacidosis, bicarbonaturia occurs and resolves metabolic alkalosis, unless the kidney’s ability to excrete HCO 3 – is impaired. If you treat organic acidoses such as lactic acidosis or ketoacidosis, ketones and lactate are metabolized to HCO 3 – and add to ECF HCO 3 –. A lesser degree of alkalosis is observed when blood anticoagulated with citrate dextrose A formula (ACD-A) is used. Similarly, large amounts of HCO 3 – precursors might be administered during massive blood transfusion or plasmapheresis. If your patient receives exogenous NaHCO 3orally for indigestion or intravenously during cardiopulmonary arrest, it adds HCO 3 – to the ECF, and can result in metabolic alkalosis. What is the cause of acid loss or alkali gain? With severe metabolic alkalosis, one should rely on measurements of arterial pH and PaCO 2 to calculate serum bicarbonate concentration.
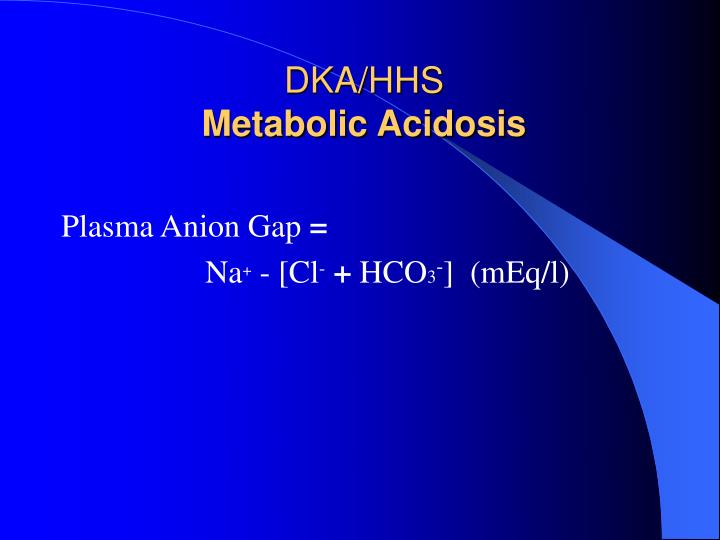
Step 5: Remember a caveat to laboratory data interpretation. Some clinical scenarios where mixed disturbances can occur are in the patient with renal failure and vomiting or the patient with diabetic ketoacidosis and vomiting. This is where ΔAG/Δ HCO 3 –ratio becomes useful in the review of your patient’s laboratory data. If the decrease in HCO 3 –is much larger than the increase in the anion gap this suggests that both an anion gap and non-anion gap metabolic acidosis are present. The increase in anion gap should roughly match the decline in HCO 3 –. Step 4: If the anion gap is elevated, compare the increase in the anion gap to the decline in HCO 3 –. One needs to keep in mind, however, that a slight increase in the anion gap is often seen in the patient with severe metabolic alkalosis due to changes in the net anion charge and increased production of organic acids. This will help identify whether an elevated anion gap acidosis is also present. If compensation is not appropriate (the change in PaCO 2 is either higher or lower than expected) then a superimposed respiratory acidosis (PaCO 2 higher than expected) or alkalosis (PaCO 2 lower than expected) is present. Remember that for each 1 mEq/L rise in HCO 3 –, PaCO 2 rises about 0.7 mmHg (range 0.6-1.0 mmHg). Step 2: Assess whether compensation is appropriate. A normal arterial pH with an abnormal PaCO 2 and HCO 3 –is a priori evidence of a mixed disturbance. Compensation attempts to return arterial pH to normal but does not quite get there. The arterial pH will be elevated in the former and low in the latter. An elevated serum HCO 3 –could be the result of metabolic alkalosis or may represent compensation for respiratory acidosis. Step 1: Assess the arterial pH and identify the primary disturbance. Factors that facilitate bicarbonaturia are adequate extracellular fluid (ECF) volume, dietary salt intake, potassium balance and appropriate mineralocorticoid activity. Most often, the kidneys can excrete excess HCO 3 – and bicarbonaturia occurs. The kidney plays a crucial role in maintaining HCO 3 –. H + loss that results in addition of HCO 3 – to the body. For each 1 mEq/L rise in HCO 3 –, PaCO 2 rises about 0.7 mmHg (range 0.6-1.0 mmHg).īased on the history, one can assess whether an increase in HCO 3 –is due to oral or intravenous alkali administration vs. In simple metabolic alkalosis the resultant compensatory alveolar hypoventilation leads to an increase in arterial carbon dioxide content (PaCO 2).

The brainstem is sensitive to interstitial and cellular H +changes and the decline in H +with metabolic alkalosis inhibits ventilation (respiratory compensation).

Metabolic alkalosis is due either to a gain in bicarbonate or a bicarbonate precursor (HCO 3 –), loss of hydrogen ion (H +) or the loss of fluid that contains Cl – in higher concentration and bicarbonate in lower concentration than serum. Does this patient have metabolic alkalosis? How does one make the diagnosis of metabolic alkalosis and differentiate simple from mixed disturbances?


 0 kommentar(er)
0 kommentar(er)
